Hi, I’m Dr. Chad Larson. If there’s anything good that comes out of a pandemic, it’s that we really accelerate our understanding of how these pathogens interact with our immune systems. If you remember the HIV/AIDS era, there was a massive increase in research and understanding of the interaction between humans and pathogens such as viruses. And from that there’s a real, accelerated learning of how our immune systems interact with them, and all the nuances and the depth and complexity of the immune system.
Now a similar thing is happening with the current pandemic virus, and there’s just a ton of research bringing out a lot of new information about how our immune systems and other things influence our risk of a worsening outcome with this particular virus. What we’re understanding is that preexisting conditions really, truly matter.
Current statistics from the CDC website say that 94% of those who are hospitalized with a severe outcome of the virus have on average 3.8 underlying health conditions, or nearly four underlying conditions. We’re talking about obesity, hypertension, diabetes, these kinds of things. And we’re understanding that this sort of acute infection on top of a chronic illness is a major accelerator to a worsening outcome. More and more studies are coming out to try and explain why that is.
I recently read an interesting study that was just published in a journal called Endocrinology, the journal of the Endocrine Society. That’s actually a great place for this particular information to be published because we already understand that endocrinology is the context for so much metabolic illness, these underlying comorbid conditions that can accelerate a person’s severe reaction to this virus. Endocrinology is underlying all of that, and the endocrine system, which is basically our hormone system, influences inflammation and our immune system overall. We’re learning that inflammation is really at the heart of it. But what’s the interaction? How do metabolic syndrome and chronic metabolic conditions influence inflammation? How does all this influence the immune system?
In this recent article, the finding is that increased inflammation results in a whole cascade of inflammatory chemicals that influence the balance, health, and reactions of the immune system. There’s a relatively new term being used now: meta-inflammation. It’s about metabolic syndrome-type inflammation.
-Dr. Chad Larson
This is an unhealthy, dysregulated type of inflammation. We’re coming to understand that this metabolic inflammation is quite significantly increased in people who are obese or overweight. Statistically, somewhere around 30 to 40 percent of the U.S. adult population is obese. And depending on what you read, something like 70 to 80 percent of the population is overweight. So a pretty large percentage of the country’s population has this potential for meta-inflammation.
How does meta-inflammation affect a person’s outcome if they get infected with this virus? There’s a couple of interesting things indicated in this research. One is the concept of a cytokine storm. Early on a lot of people were talking about this. Although I’m not hearing as much about it any more, it’s definitely a common feature among those who get a more severe outcome of the virus. So, what is a cytokine storm?
Cytokines are a group of inflammatory chemicals. We call them cytokines and chemokines. But there are a few specific ones that seem to be particularly implicated in a worsening outcome of COVID. One of them is called interleukin 6, or IL-6. IL-6 is one of the cytokines that really seems to be majorly upregulated in somebody who has a combination of meta-inflammation from obesity or other metabolic condition combined with the pandemic virus. In these circumstances there’s already a little bit of inflammation, which is understood to be common in people with metabolic syndrome. But when they get infected with a virus, there can be a massive increase in interleukin 6. In fact, studies show that an interleukin 6 of greater than 80 picograms per milliliter had a twenty-two-fold increase in respiratory failure. In other words, the respiratory system was so compromised that the person had to be hospitalized. A twenty-two-fold increase is over two thousand percent greater chance, if the interleukin 6 is above 80 picograms per milliliter. That’s a really strong correlation between this type of inflammation and a worsening outcome of COVID.
That’s the inflammatory system, but how does this influence the immune system? Part of the same inflammation/dysregulation is that a very specific part of the immune system gets involved. If you have typical blood work done, part of it is going to include the CBC, the complete blood count. There are the red blood cells and white blood cells, and we have another section called the differentials. The differentials are basically your five main white blood cells: your neutrophils, lymphocytes, monocytes, eosinophils and basophils.
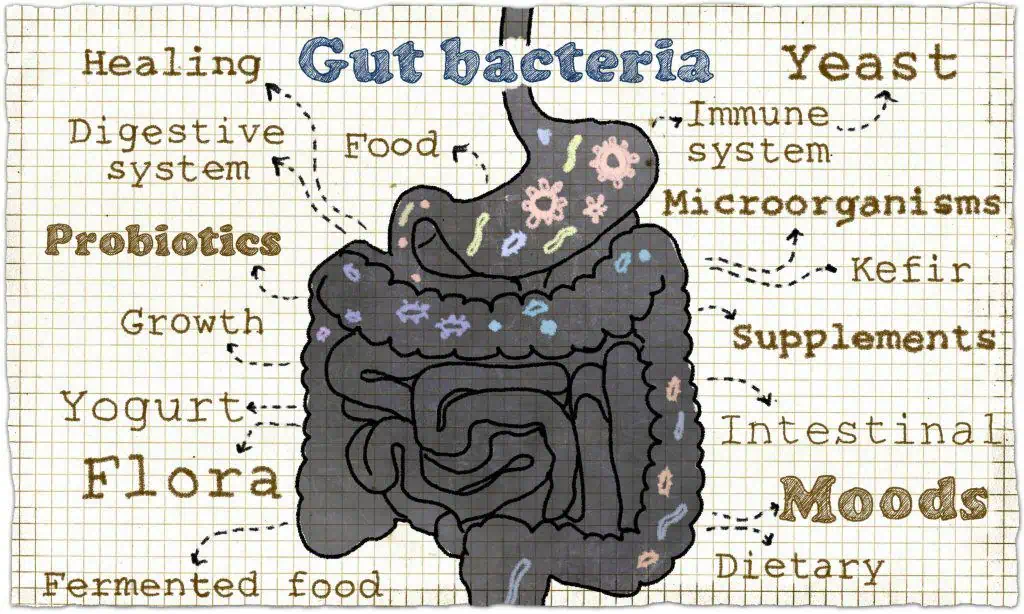
Monocytes are a key part of your immune system and they differentiate or morph into another substance called a macrophage. Macrophage means “big eater.” So if we have a pathogen, a bacteria or virus in the system, a macrophage will eat it, will gobble it up, and will get rid of it. Part of the job is just to get rid of that pathogen, but another part of the job is that the macrophage becomes what we call an antigen presenting cell. It says, “hey, check out this virus I just gobbled up. Maybe we should do something about this.” And that eventually could cause the T-cells and B-cells to produce antibodies. This is part of the process of how antibodies are produced, starting from that macrophage.
So, this is all good. This is all normal. This is part of a healthy process. However, there are two different forms of macrophage: M1 and M2. M2 is actually anti-inflammatory, a good healthy balancing type of macrophage.
But if we have too much of the M1 type of macrophage, this is a very pro-inflammatory process. So this collision of the immune system with the inflammatory system goes basically like this. An individual has metabolic syndrome or one of these metabolic conditions, so that there’s already an undertone of dysregulated inflammation imbalance. Combining that imbalance with a virus causes the macrophages, which are part of your immune system, to dysregulate. This could easily lead to the kind of inflammatory cytokine storm that can eventually infiltrate the upper respiratory system. And that’s one way somebody could have a severe outcome of the pandemic virus.
The real takeaway of the study was that these preexisting conditions really matter. The whole metabolic syndrome meta-inflammation is actually the underlying factor in a vast majority of pandemic patients who have a worsening outcome. So, preexisting conditions matter greatly.
You should really look to maximize your metabolic health because the pandemic virus is more endemic at this point. It’s going to be part of our reality, part of our culture. And so the message is really to emphasize just how important it is to maximize, improve, and optimize your metabolic health. I will keep reading the studies and bringing you the information. Until then, keep it real.